Test will try to fend off type 1 diabetes
By Warren King
Thursday, November 24, 2005
Seattle Times medical reporter
Seattle researchers will soon begin testing a way to stave off diabetes by tripping up the immune system with the help of mouse cells.
Scientists at the Pacific Northwest Research Institute (PNRI) will be part of a national effort to see if they can stop type 1 diabetes — or at least delay its progression — by derailing the immune cells that attack the body's insulin producers.
The experimental therapy "has a reasonable shot at being the first building block toward a cure," said Dr. Bill Hagopian, director of PNRI's work on the therapy. In early trials, the treatment has enabled patients to continue making a portion of the insulin they need for up to two years.
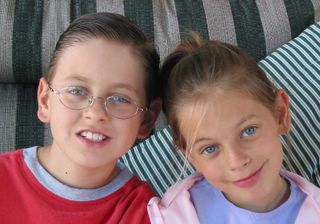
Type 1 diabetes, formerly known as juvenile diabetes, afflicts more than 1 million people in the United States. It develops when the immune system destroys the cells that produce insulin, which the body needs to process sugar.
Most cases of type 1 diabetes develop in childhood or young adulthood, and patients become dependent on injected insulin for the rest of their lives. Complications include heart disease, stroke, blindness, kidney damage and amputations. Many sufferers have shortened lives.
Scientists in Seattle and four other cities are testing the notion that if they treat patients within about six months of a diabetes diagnosis, they can prevent destruction of all the insulin-producing "beta" cells.
"We want to get in there early to extend the 'honeymoon' phase," when about 10 percent to 25 percent of the patient's beta cells are alive and still functioning, Hagopian said.
Diabetes study
To learn more, including how to enroll, call the Pacific Northwest Research Institute, 888-324-2140, or Benaroya Research Institute, 800-888-4187.
The treatment would not be effective for the more-common type 2 diabetes, which usually begins in adulthood and affects more than 19 million people in the United States. It is not caused by an immune-system problem but develops when the pancreas gradually loses its ability to produce insulin.
Researchers at PNRI will test the type 1 treatment on 13 newly diagnosed patients, ages 15 to 30. They will be among a total 70 patients nationwide, including at Columbia University; the University of California, San Francisco; the University of Colorado; and the University of Florida. The Benaroya Research Institute at Virginia Mason Medical Center in Seattle also is planning to join the study, funded by the National Institutes of Health.
And that's where the mice come in.
The treatment relies on the rodents to help make a drug containing the protective antibodies:
These "monoclonal antibodies" are taken from laboratory-preserved mouse cells, then altered to prevent a human allergic reaction and tailored to seek out key human immune cells.
The antibodies then are mass-produced and injected into the patients, where they "neutralize" the immune cells that otherwise would orchestrate a wide attack on the insulin-producing beta cells.
Scientists believe that protecting those remaining beta cells will decrease the chances of long-term complications of diabetes, especially with repeated treatments. They also hope that the therapy eventually may "reset" the immune system, permanently ending the attacks on beta cells.
In a best-case scenario, the beta cells then would begin to multiply slowly, perhaps with the help of hormonal treatments, and eventually return to normal levels, essentially curing the diabetes, Hagopian said.
To read the rest of the Article go to Seattle Times Local News